Schedule M 1 of drugs and cosmetics rules explains the GMP requirements for Homeopathic industry in India. It defines Good Manufacturing Practices and requirements of premises, plant and equipment for Homeopathic medicines. Schedule M came into effect in 1987. Amended schedule M was notified in 2006.
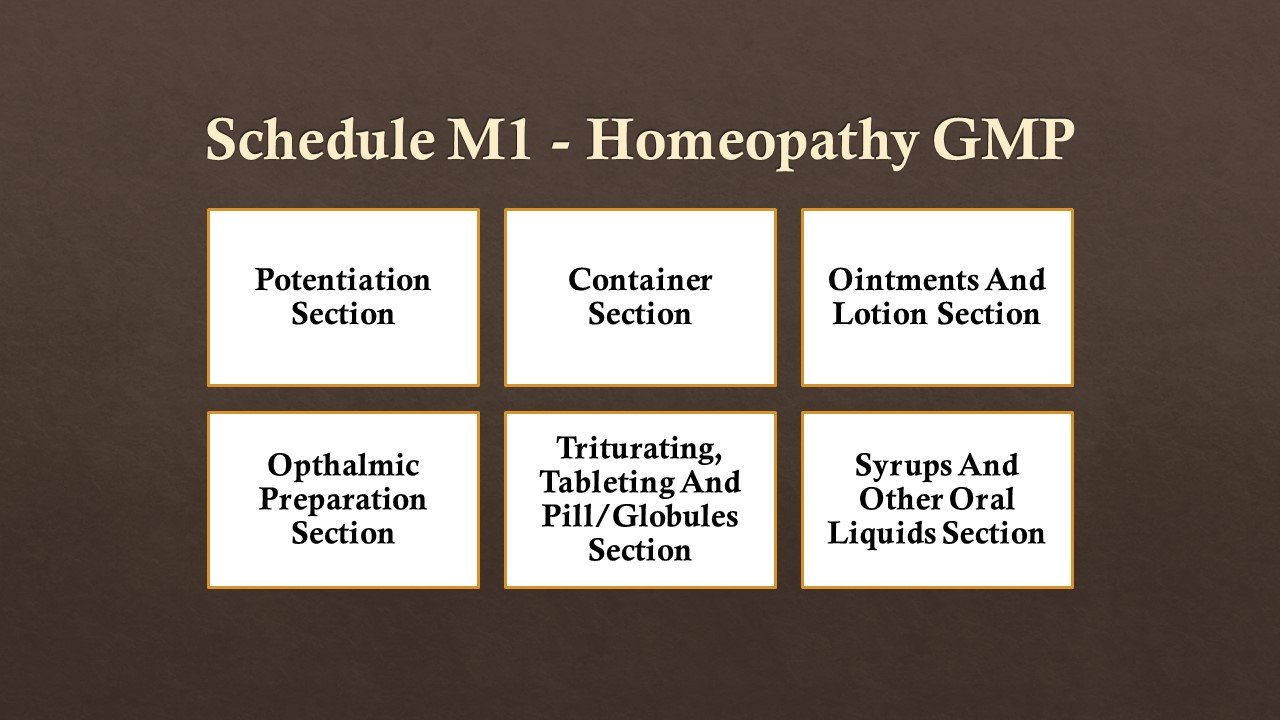
Schedule M is titled as “Good Manufacturing Practices And Requirements Of Premises, Plant And Equipment For Homoeopathic Medicines“. Schedule M1 has following sections:
GENERAL REQUIREMENTS
1.1 Location and Surroundings: – The premises shall be situated at a clean place which shall not be adjacent to open drains, public lavatory or any factory producing pollution of any kind, garbage dump, slaughter house or any other source likely to cause contamination from the external environment. The premises shall be located away from railway lines so that the performance of sensitive electronic equipment is not affected by vibrations. There shall be no open drains inside or outside the manufacturing premises. It shall be so designed that the entry of rodents is checked. The drains shall facilitate easy flow of the effluent and shall be cleared periodically.
1.2 Building: – The premises shall not be used for any purpose other than manufacture of homoeopathic drugs and no part of the manufacturing premises shall be used for any other purpose. Other facilities, if needed, could be provided in separate building(s) in the same campus. Crude raw materials, packing materials, etc. shall be stored and handled in places earmarked for them and shall not be taken inside areas where critical operations of manufacture are done excepting processed raw material. Heating, washing, drying, packing and labelling etc. wherever needed, shall be done in dedicated ancillary areas adjacent to the manufacturing sections concerned. The walls and floorings of manufacturing areas shall be smooth and free from chinks, cracks and crevices and shall be washable. The design of the windows, windowpanes and all fittings shall be such that they will not facilitate accumulation / lodging of dust and other contaminants.
PLANT AND EQUIPMENT
2.1 General: – The design of the plant shall be suitable for the nature and quantum of the activities involved. Equipment shall be installed in such a manner as to facilitate easy flow of materials and to check criss-cross movement of the personnel. The entry to all manufacturing sections shall be regulated and persons not associated with the activities in the sections shall not have access to them. There shall be arrangements for personal cleanliness of workers and toilets. These shall be separate for men and women workers. There shall be suitable arrangement, separate for men and women, to change from their outside dress and footwear into the factory dress and footwear. Uniforms of suitable colours and fabric which facilitate proper washing and which do not shed fibres other contaminants shall be provided. Suitable head-covers and gloves shall be provided to the workers. The manufacturing premises shall not be used for dining. There shall be separate area for the personnel to take food or rest. Toilets shall be located in or adjacent to any of the areas concerned with any manufacturing activity. Spitting, smoking, chewing, littering, etc. in the manufacturing or ancillary areas shall not be permitted. Standard operating practices (SOPs) for cleaning and sanitation, personal hygiene of the workers, general and specific upkeep of the plant, equipment and premises and every activity associated with manufacture of drugs including procurement, quarantine, testing and warehousing of material shall be written and adopted. No person with any contagious disease shall be involved in any of the manufacturing activities.
There shall be proper arrangements for maintenance of the equipment and systems. The performance of every equipment and system shall be properly validated and their use shall be monitored. Dos and don‘ts in the matter of the use of the plant and equipment as may be applicable shall be written and displayed in all places.
There shall be separate dedicated areas for each ancillary activity such as receipt, cleaning, warehousing and issue of raw materials, packaging materials, containers and closures, finished goods etc. Adequate measures shall be taken to prevent entry/presence etc. of insects, rodents, birds, lizards and other animals into the raw material handling areas. Every material shall have proper identification and control numbers and inventory tags and labels displaying status of the quality being used, etc. There shall be proper arrangements and SOPs for preventing mix-up of materials at every stage of handling. There shall be separate arrangements for handling and warehousing of materials of different origins.
Materials with odour shall be kept in tightly closed containers and shall be well protected from other materials. Fresh materials and odorous materials shall, preferably be stored in separate dedicated areas. Where bonded manufacturing and / or warehousing facilities are required as per Excise laws, the facilities required shall be provided without compromise on the requirements specified above.
A well equipped laboratory for quality control/quality assurance of raw materials and finished products and for carrying out in-process controls shall be provided.
(a) Rooms: – The rooms shall be airy, ventilated, and maintained at temperatures which are moderate and comfortable. Sections which are required to be sterile, air-conditioned and provided with air handling system shall be designed accordingly. All sections shall be free from insects, birds, rodents, worms etc. and suitable measures shall be taken to prevent the same from finding ways to the sections and equipment.
(b) Water: – The water used for manufacture of drugs shall be of the quality as prescribed in the rules or in the Homeopathic Pharmacopoeia concerned, as the case may be, and shall be prepared from pure drinking quality water, free from pathogenic organisms.
(c) Disposal of waste: – Effluents, organic and inorganic wastes shall be disposed of in such a manner as may be prescribed in the laws pertaining to pollution control and if no such law exists in the place of manufacture, they shall be rendered harmless and shall be disposed of in such a manner that they are not hazardous to health of the public or cattle or plants.
(d) Factories Act: – The provisions of the Factories Act, 1948(Act 63 of 1948), as applicable shall be adhered to.
(e) Medical Services:- All persons concerned with any activity pertaining to manufacture of drugs including handling of raw materials, packing materials, packing and labelling of drugs, etc. shall be medically examined for fitness at the time of employment and subsequently at periodic intervals and records thereof shall be maintained.
(f) Safety measures: – First-aid facilities shall be provided in such a manner that they are easily accessible and staff shall be imparted knowledge and training in first-aid measures as may be needed. Fire control equipment in suitable numbers shall be provided at easily accessible places near all sections including stores and warehouses.
(g) Workbenches: – Workbenches suitable to the nature and quantum of the work involved shall be provided in all sections. Such work benches in general, shall have smooth, washable and impervious tops and the parts shall not be rough or rusty or damaged otherwise.
(h) Container management: – Proper arrangements shall be made for receiving containers, closures and packing materials in secluded areas and for de-dusting the same, removal of wastes, washing, cleaning and drying. Suitable equipment shall be provided as may be needed, considering the nature of work involved. Where soaps and detergents are used to wash containers and closures used for primary packing, suitable procedure shall be prescribed and adopted for total removal of such materials from the containers and closures.
Plastic containers which are likely to absorb active principle or which are likely to contaminate the contents may not be used.
Glass containers used shall be made of neutral glass. The closures and washers used shall be of inert materials which shall not absorb the active principles or contaminate the contents or which may otherwise be likely to cause deterioration of quality.
The containers, closures and packing materials shall protect the properties of the medicines, Tablets, if blister-packed, shall have secondary protective packaging to protect the medicines from moisture, odour etc. Neutral glass phials and epoxy-coated closure shall be used for eye-drops. Transparent plastic containers may be used for eye-drops containing only aqueous preparations. Sterile plastic nozzles may be provided to eye-drops separately along with the medicine, whatever needed.
2.2. Personnel– Manufacture of drugs shall be under the control of approved technical staff that shall possess the qualifications prescribed in rule 85.
REQUIREMENT OF EQUIPMENT AND FACILITIES
3.1. Mother tinctures and mother solutions:– The following equipment and facilities shall be provided:-
(i) Disintegrator;
(ii) Sieved separator;
(iii) Balances, weights and fluid measures, all in metric system;
(iv) Chopping table/board and knives;
(v) Macerators with lids (all made of stainless steel of grade 304 or neutral glass);
(vi) Percolators (all made of stainless steel of grade 304);
(vii) Moisture determination apparatus;
(viii) Filter press/Sparkler filter (all metal parts shall be of stainless steel);
(ix) Mixing and storage vessels (Stainless steel of grade 304);
(x) Portable stirrers (Rod, blades and screws shall be of stainless steel);
(xi) Water still/water purifier;
(xii) Macerators and percolators for preparing mother solutions of materials of chemical origin. These shall be of material, which will not react with the chemicals, used and which do not bleach; and
(xiii) Filling and sealing machine.
The area and facilities for manufacture of mother tinctures and mother solutions shall be separate and shall be 55 square meters for each for basic installations.
3.2. Potentisation section:– The section shall have the following facilities:-
(i) Work benches with washable impervious tops;
(ii) Facilities for orderly storage of different potencies and back-potencies of various drugs;
(iii) Suitable devices for measuring and dispensing of potencies/back-potencies into the potentisation phials;
(iv) Potentiser with counter.
An area of 20 square meters shall be provided for basic installations.
Note: –
(a) The requirement of potentiser is not mandatory. The process may be done manually also with proper SOPs. Potentiser, if used, shall be properly validated and shall be calibrated every time before commencement of work for proper performance.
(b) The manufactur er sh all use back-poten cies procur ed fr om Licen sed
manufacturers and the firm shall maintain proper records of purchase or shall prepare own-back potencies . Every container of potencies and back-potencies shall be kept properly labelled and there shall not be mix-up of different medicines and different potencies.
3.3. Containers and Closures Section: – Separate area for preparation of containers and closures shall be provided adjacent to the potentisation section. This area shall have the following facilities:-
(i) Washing tanks with suitable mechanical or hand operated brushes;
(ii) Rinsing tanks. Purified water shall be used for rinsing;
(iii) Closures washing / macerating tanks;
(iv) Driers;
Note: –
(a) Different droppers shall be used only for each different medicine and different potency.
(b) All measures shall be in metric system. Measures used shall be of neutral glass. Metal droppers and plastic droppers shall not be used.
(c) Glass droppers shall be reused only after proper cleaning and sterilization
(d) Potentisation shall be done by the method(s) prescribed in the Homoeopathic Pharmacopoeia of India.
3.4. Trituration, Tableting, Pills and Globules making sections:– The following basic equipment and facilities shall be provided:-
(i) Triturating Machine;
(ii) Disintegrator;
(iii) Mass Mixer;
(iv) Granulator;
(v) Electrical Oven;
(vi) Tablets punching Machine;
(vii) Kettle (steam or electrically heated ) for preparing solutions;
(viii) Driers for drying granules and tablets;
(ix) Sieved separator (stainless steel);
(x) Tablet counter;
(xi) Balances;
(xii) Coating Pan with spray-gun;
(xiii) Multi-sifter
(xiv) Mill with perforations.
An area of 55 square meters shall be provided for basic installations. The area shall be suitably divided into cubicles to minimize cross contamination, mix-up etc.
Note: – The section shall be free from insects, worms, rodents, dust and other floating particles and moisture.
3.5. Syrups and other oral liquids section:– The following basic equipment and facilities shall be provided:-
(i) Mixing and storage tanks (stainless steel of grade 304);
(ii) Portable stirrer (rod, blades and screws shall be of stainless steel);
(iii) Filter press / Sparkler filter (all metal parts shall be of stainless steel);
(iv) Filling and sealing machine;
(v) pH meter.
An area of 20 square meters shall be provided for basic installations. The section shall be free from dust and other floating particles, cobwebs, flies, ants and other insects, birds, lizards and rodents.
(1) Adequate number of workbenches shall be provided.
(2) Visual inspection table shall be provided. This shall comprise of a colour con trast backgr ound with lamp for providing diffused light, mounted on a suitable table.
3.6. Ointments and lotions section:– The following basic equipments and facilities shall be provided:-
(i) Mixing tanks (Stainless steel)
(ii) Kettle (steam or electrically heated) for preparing solutions
(iii) Suitable powder / planetary Mixer
(iv) Ointment mill / colloidal Mill / Emulsifier
(v) Filling and sealing machine / Crimping machine
(vi) Filtering equipment
(vii) Balance and weights
A minimum area of 20 square meters shall be provided for basic installations. An ancillary area for washing vessels and equipment shall be provided. An ancillary area for heating purposes shall also be provided.
3.7. Ophthalmic preparations section:– The following basic equipment and facilities shall be provided:-
(i) Hot air oven, electrically heated, with thermostatic control;
(ii) Laminar Air Flow bench;
(iii) Air Handling Unit with HEPA filters to provide filtered air and positive pressure to the section and air-locks;
(iv) Ointment mill / colloidal mill;
(v) Mixing and storage tanks (Stainless steel of grade 304);
(vi) Pressure vessels, as may be needed;
(vii) Sintered glass funnels, Seitz Filter / Filter candle;
(viii) Vacuum pump;
(ix) Filling machines for liquids ointments etc.;
(x) Autoclaves with pressure and temperature gauges; and
(xi) Necessary workbenches, visual inspection bench, etc.
Area: Minimum area of 20 square meters shall be provided for basic installations.
Note: –
1. The section shall have a clean room facility of Class 100 specification.
2. The section shall be air-conditioned and humidity controlled.
3. Entry to the sections shall be regulated through air-locks with differential air pressures with the air-lock adjacent to the section having higher pressure and the first one through which entry is made with the least pressure.
4. Materials shall be passed to the sections through suitable hatches.
5. The personnel shall wear sterile clothing including headgear, which shall not shed fibre.
6. Washing of phials shall be done in separate areas with proper equipment. Proper facilities shall be provided in the area for washing vessels.
7. Separate area shall be provided for packing and labelling.
QUALITY CONTROL DIVISION
4.1. Functions:– A separate quality control division shall be provided in the premises. The section shall be under the control of an approved technical officer, independent of the manufacturing division and directly responsible to the management. The section shall be responsible for ensuring the quality of all raw materials, packing materials and finished goods. The section shall also carry out in-process quality checks of the products. The section shall be responsible for the stability of the products and for prescribing their shelf life wherever applicable.
The functions of the division shall include:-
(1) To test the identity, quality and purity of the raw materials and to recommend rejection of the material of poor quality and approve materials of the prescribed quality only.
(2) To test the identity, quality and purity of the finished products and to recommend rejection of the material of poor quality and to approve materials of the prescribed quality only.
(3) To prepare and validate the methods of analysis, validate the equipment,
monitor their use, take steps for proper maintenance, etc.
(4) To approve or reject container s, closures and packaging materials in accordance with the prescribed norms.
(5) To exercise / carry out in-process control of products.
(6) To prescribe SOPs on all matters concerning quality of materials and products.
(7) To monitor the storage and handling of raw materials, finished products,
containers, closures and packaging materials.
(8) To investigate complaints on quantity of products and take / recommend appropriate measures and to examine returned goods and recommend their proper disposal.
4.2. Personnel:– The quality control staff shall be full-time personnel. Analysis and tests of drugs, raw materials, etc. shall be done by qualified and approved technical staff. The technical staff shall have the minimum qualification of degree in Homoeopathic Pharmacy or Science with Chemistry or Botany as the principal subject and experience of not less than two years in the test and analysis of medicines including handling of instruments.
4.3. Equipment: – The following equipment shall be provided:-
(i) Microscope of suitable magnification and photographic device;
(ii) Dissecting microscope;
(iii) TLC apparatus;
(iv) UV lamp viewer;
(v) Monopan Digital Electronic Balance;
(vi) Hot air oven;
(vii) Distillation apparatus;
(viii) Water Bath;
(ix) Polarimeter;
(x) Refractometer;
(xi) Melting point apparatus;
(xii) pH meter;
(xiii) Magnetic stirrer;
(xiv) Table Centrifuge;
(xv) Muffle furnace / electric Bunsen;
(xvi) Moisture determination apparatus;
(xvii) U.V. Spectrophotometer;
(xviii) Rotary microtome / Section cutting facilities;
(xix) Tablet Disintegration Machine.
RAW MATERIALS
5.1. Raw materials of Plant Origin:–
(a) The raw materials of plant origin used for manufacture of drugs shall be of the following specifications:-
(i) the materials shall be those recently collected and dried and shall be free from moisture so as to eliminate the risk of deterioration and infestation with pests moulds, etc. The materials shall be collected when the atmospheric temperature is suitable where its active constituents are not changed / damaged / destroyed.
(ii) when fresh materials are to be used, the time lapse from the time of collection to use shall be minimized to the extent possible;
(iii) the materials should be taken from healthy plants and shall be free from parasites, moulds, etc.;
(iv) the materials shall be free of inorganic or organic foreign matter;
(v) when dry materials are procured, they shall be from healthy plants and shall be in unprocessed form, free from all extraneous matters such as fungus, insects, moulds, pathogenic organisms, etc. and should not be more than six months old. Plant materi alsof Agaricaceae, which are perishable shall be used within one week of collection.
(b) To facilitate proper identification and purity of the material and to exercise proper quality control of the material, the following conditions must be satisfied:-
(i) a small twig of the plant with leaves shall be available if the part used is bark of the plant;
(ii) an entire plant or part or aerial twig with leaves and some uncut roots / rhizomes / bulbs shall be available if the part used is a root /rhizome / bulb;
(iii) if plants with flowers are to be used, a few dry flowers shall also be available with the aerial twig;
(iv) if the material used is a mould or of the plant families Agaricaceae, Polyporaceae/ amanitacaea / Boletaceae / Russulaceae, a whole specimen plant / mould shall be available in properly dried form;
(v) the materials shall be free from insecticides, fungicides, etc;
(vi) the materials shall be in open mesh bags or in suitable material which permits the passage of air inside;
(vii) each consignment of the material shall be accompanied by a statement of the supplier‘s name; name of the plant with description of the part supplied. The pharmacopoeial reference, place of collection /harvest, date and time of collection and packaging and weight.
5.2. Raw material of Chemical origin: – They shall be of respective pharmacopoeial standards and statements of their specification shall accompany the materials.
5.3. Raw materials of animal origin: – The materials shall be those collected from healthy animals and shall be of pharmacopoeial specifications. The materials shall be those collected, packed and transported under proper hygienic conditions and well protected from all contamination. The materials shall be accompanied by statements as in para ‗a‘ above. In case of drugs derived from a whole insect, bulk of such drugs along with some uncut whole insect should be provided / maintained for records.
5.4. Sarcodes: – The materials shall be those collected from healthy animals and shall be of pharmacopoeial specification. The materials shall be those collected, packed and transported under proper hygienic conditions and well protected from all contamination. The materials shall be accompanied by statements as in the Para ‗a‘ above. The materials shall be tested to see that they are free from pathogenic organisms such as E. Coli, Salmonella, etc.
5.5. Nosodes: – These shall be of pharmacopoeial specifications. As these are derived from diseased animals or human beings, they shall be autoclaved immediately after collection and preserved and transported under proper hygienic conditions and well protected from all contamination. Before use, these shall be sterilized by autoclaving and shall comply with the test for sterility as specified in the Homoeopathic Pharmacopoeia.
PROCEDURES
6.1. Manufacture of Mother tinctures: –
(a) Every material shall be identified and checked for its purity. They shall be cleaned and processed by cutting, chopping, etc. for use in macerators / percolators. A specimen of the material shall be preserved till approval of the product for release for sale.
(b) The design and procedures adopted shall ensure reproduction of the product of the same quality every time.
(c) Mother tinctures shall be preserved in tight closed neutral containers at temperatures preferably below 250 C, protected from light.
6.2. Manufacture of Attenuations: –
(a) Attenuations shall be prepared in a clean room environment with filtered air and positive pressure inside suitable for the operations.
(b) The methods used shall be reproducible and shall be validated.
(c) The containers, tubings, etc. of the machines used for manufacture of attenuations shall be thoroughly washed, cleaned and dried after attenuation of a drug. Regular checks shall be carried out on the materials.
(d) The parts of the equipment that come into contact with the attenuation materials shall be of neutral quality and shall not cause any contamination to the material.
(e) Attenuations shall be preserved in properly labeled glass containers.
(f) Alcohol and other vehicles used shall be of Homoeopathic pharmacopoeia specification and shall be free from impurities.
6.3. Trituration: – Trituration technique is used to manufacture drugs from insoluble strains. The procedure / method specified in the Homoeopathic pharmacopoeia shall be adopted.
6.4. Formulations:– Compound formulations shall preferably be in liquid and solid forms and the potency of the ingredients shall be in detectable quantity preferably be in 3x except in case of highly poisonous material and toxins which should not be below 6x. The ingredients shall be compatible to each other. Complete pharmacopoeial name of each ingredient shall be printed on the label along with composition.
6.5. Medicated Insert Pellets: –
(a) Pellets shall be manufactured in clean rooms free from particulate contaminants. The equipment used shall enable prevention of contamination and cross- contamination.
(b) The procedures shall be validated.
LABORATORY CONTROLS
Tests as per the pharmacopoeia and requirements shall be carried out on products and materials. The stability of the products shall be established by proper methods. Sterility tests, wherever applicable, shall be carried out. Control samples shall be preserved for not less than three years after the last sales.
PACKING AND LABELLING
A minimum area of 50 square meters shall be provided for packing and labeling section.
EXPIRY DATE
Not exceeding sixty (60) months from the date of manufacture.
STANDARD OPERATING PRACTICES
Standard Operating Practices (SOPs) shall be developed for various activities such as receipt, identification, cleaning, drying, warehousing, issue, handling, sampling etc. of all materials. Labels and packing materials shall be examined for correctness and compliance with rules. Records shall be maintained for their printing, use, destruction etc.
RECORDS AND REGISTERS
Records shall be maintained for all the activities. These shall include records of production, records of raw materials, records of testing, records of sales and other supplies, records of rejection, complaints and actions taken, SOPs and records in respect of compliance thereof, log books of equipment, master formula records, records of medical examination and fitness of personnel etc. All records shall be maintained for a period of one year after the expiry of a batch or for three years whichever is later.
Download Schedule M1 pdf: Download Schedule M, M1, M2, M3 GMP Pdf
Schedule M, Schedule M2 and M3 are different from Schedule M1.
Visit Here For Difference Between Schedule M, M1, M2, M3 GMP, Drugs & Cosmetics Act
You should note that Schedule M, M1, M2, M3 define good manufacturing practice for India.
However if target market is USA and Europe then pharmaceutical Industry need to follow the USFDA cGMP and ICH Guidelines.
If target market is mostly developing countries then WHO GMP guidelines are followed in most of them.
You May Also Like:
Difference Between Schedule M, M1, M2, M3 GMP, Drugs & Cosmetics Act

